Urinary Tract Infection
Incidence
Urinary tract infections (UTI) in women are extremely common. Between 30 and 50% of adult women will suffer with a urinary tract infection in their lifetime. The prevalence rate for having one episode of UTI in a given year varies from 8% to 10% and result in 7 million consults at General Practice annually. After the first infection 25% of women will have a second infection within 3–6 month. In contrast, urinary tract infections in men and children are rare, and ANY infection in these patients merits full investigation.Recurrent UTIs:
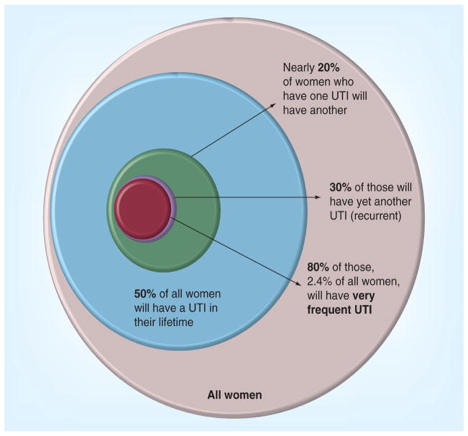
Recurrent UTIs are defined as >3 culture confirmed infections in 1 year or >2 in 6 month period. Recurrent infections can be due to RELAPSE when they occur within 2 weeks of an earlier UTI with the same bacteria or RE-INFECTION when they occurs >4 weeks after earlier UTI with a different bacteria.
Causes of UTI
Most UTIs are caused by translocation (spread) of bacteria from the bowel to the vagina and from this source up the urethra (water-pipe) to the bladder. As such most infections are caused by Coli-(colon) form bacteria. The most common of these are E. coli species, which cause 70-80% of water infections. Other causes of infections are Staphylococcus bacteria (10%) and in patients with diabetes Klebsiella, Group B streptococci and Enterococci bacteria. In elderly patients infections with multiple different bacteria become more common.Risk factors of UTI
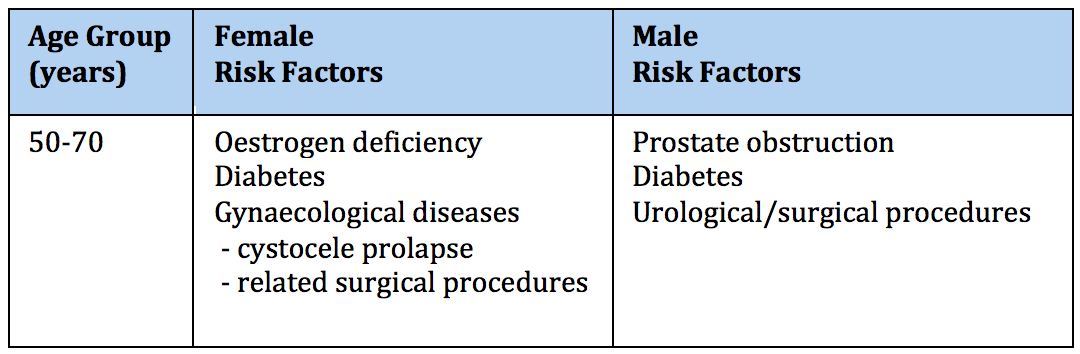
Several factors increase the risk of UTI. These can be separated into several categories that often co-exist:Colonisation of vagina and urethra
- Hormone deficiency especially after menopause causes vaginal atrophy (thinning)
- Spermicidal jelly increases vaginal pH
- Antibiotics reduce vaginal lactobacilli (the natural bacteria of the vagina that prevent colonisation by other bacteria)
Ascent to bladder
- Short urethral length (this is a rare congenital problem)
- Sexual milk back
- Catheterisation pushes bacteria into the bladder causing colonisation of the bladder. In patients who use regular catheters a urine culture will always test positive for bacteria
Establishment of bacteria in bladder
- Urine composition (extremes inhibit bacterial growth)
- Reduced antibody (IgA and IgG antibodies)
- Reduced glycosamine glycan (GAG) layer in the bladder. This is the natural mucus produced by the bladder lining to prevent bacteria adherence and penetration into the lining cells
- Low urine flow
- Incomplete bladder emptying
Symptoms and Signs
Urinary tract infections may cause local irritation (cystitis) or systemic symptoms- Bladder Symptoms are urinary frequency, pain, lower abdominal discomfort and urine odour
- Systemic symptoms are fever and loin pain if the infection ascends up to the kidneys
Diagnosis of UTI
Your consultant will take a detailed history, which should include:- The precise nature of your bladder symptoms
- Fluid and hygiene management
- A sexual history including partners and method of contraception
- Gynaecological and obstetric history
- Medication particularly anticholinergic, psychotropic, and immunosuppressive drugs
- Nitrites specificity 94%
- Leukocyte esterase specificity 74-95%
- An extended urine culture is often requested to exclude less common bacterial types
- An ultrasound of the urological tract with a measurement of the post void residual urine is used to check bladder emptying
- Targeted flexible cystoscopy (8% yield) is used for patients with recurrent or persistent UTIs or blood in the urine
Treatment of Recurrent UTIs
Behavioural Modifications
Fluid intake and Hygiene
- Increase fluid intake to 1-2 litres (drinking more than this simply increases urinary frequency)
- Double voiding techniques to ensure best bladder emptying
- Wipe from front to back to avoid transferring bacteria from colon to vagina
- Avoid skin allergens introduced to the genital area eg. bubble baths which could alter vaginal bacteria
Sexual Intercourse
- Avoid multiple partners
- Avoid before and after sexual intercourse
- Avoid spermicidal contraceptives, diaphragms and vaginal douching
- Avoid anal translocation (transfer of bacteria from colon to vagina) during sexual intercourse
Non-antibiotic prophylaxis
Non- antibiotic prophylaxis aims to avoid regular use of antibiotics. The aim is to lower the risk of antibiotics including overgrowth of fungal infections (thrush), reduce the development of antibiotic resistance for you and the wider community and reduce the cost of treatmentCranberry
Cranberry (Vaccinium macrocarpon species) use may inhibit bacterial adherence to the bladder lining, and has been advocated as a prophylaxis against UTI. Cranberry juice or tablets containing a minimum of 36mg/day proanthocyanindin A have been used in low level (III) studies. The evidence of substantive benefit is weak and current UK and international guidelines do not support their regular use.D-mannose
D-mannose is a naturally occurring sugar, found in the bladder, which binds to proteins. D-mannose binds to the type 1 pilli of bacteria and is thought to Inhibit bacterial adherence to bladder lining in a similar fashion to Cranberry. Studies are limited and international guidelines do not support D-mannose regular use.Probiotics
The vagina is naturally colonised by bacteria and particularly lactobacilli strains. It is hypothesized that administration of oral lactobacilli may boost the vaginal flora and displace colonisation of infective species. Supportive evidence for this theory is weak and currently only exists for specific strains L. rhamnosus GR-1 and L. reuteri RC-14. Current guidelines do not recommend regular use.Hipprex
Methenamine hippurate (Hipprex) has antibacterial activity because the methenamine component is converted to formaldehyde – an antiseptic- in acid urine. Hippuric acid, the other component, keeps the urine acid. The drug is generally active against E. coli, enterococci and staphylococci. Enterobacter species are generally resistant. Hiprex may benefit patients with recurring urinary tract infections when long-term therapy is considered necessary. The evidence base for this remains poor.Oestrogen Cream
There is good evidence that replenishing depleted oestrogen levels in the vagina of post menopausal women improves vaginal atrophy – thinning of the vaginal lining – and reduces the risk of bacteria ascending from the vagina up the urethra (water-pipe). Vaginal oestrogen levels can be increased by use of oestrogen creams or pessaries. Oestrogen creams can cause local irritation but systemic absorption and effect is minimal.Antibiotic Use
Bacteria can often be found in urine testing even in patients who have no symptoms. This is called asymptomatic bacteriuria. Current guidance is that asymptomatic bacteriuria does not need treatment, and treatment risks increasing antibiotic resistance developing. The exception to this is pregnancy when bacteriura is associated with increased risks to the developing foetus and mother. Bacteriuria in pregnancy should be treated.Self-start antibiotic therapy Antibiotic Use
— Bacterial eradiation at 2 days
— Treatment is 98% effective in 3-days
— Antibiotic treatment of simple UTIs reduces symptom
duration by 1-2 days versus simple measures alone.
- Early administration of antibiotics is effective at clearing uncomplicated infections within hours of being started. Whilst 1-day regimes may be insufficient, studies have shown that there is NO difference between 3 day and 5-10 day antibiotic courses.
- Antibiotic treatment should be based on the sensitivities of the bacteria isolated in urine culture. It is therefore important that a urine culture is therefore taken before antibiotics are started, and the antibiotics adjusted according to the sensitivities when obtained. If the bacteria are sensitivity to the initiated antibiotic then a 3-day course will suffice in simple cases.
Prophylactic antibiotics
Modern practise is encouraging short courses of self start antibiotics rather than long-term antibiotic use for patients with simple infections. The aim is to avoid the development of multi resistant bacteria in the patient (as well as the wider community). Long-term antibiotics are associated with altered bowel and vagina bacteria and overgrowth of fungal (thrush) infections. Prophylactic antibiotics are sometimes appropriate in patients with complex urological anatomy or bladder dysfunction.UTI Vaccines
A number of bacterial extracts have been proposed as ‘vaccines’ to stimulate the body’s natural immune response and protect against recurrent UTI. Most of these are experimental and have little evidence base.- Uro-Vaxom® is an extract (lysate) from 18 uropathogenic E. coli strains and ais administered as an oral capsule daily for 3-months, and three 10-day boosters thereafter. Early studies have suggested some benefit over placebo and the drug has been licensed in some European countries, but not the United Kingdom
- Urommune® is a sublingiual (under the tongue) spray of selected strains of Escherichia. coli (UPEC), Klebsiella pneumoniae, Proteus vulgaris, and Enterococcus faecalis). No high level evidence has been published but observational study has suggested a possible benefit. The drug is not licensed in the United Kingdom

