Cough (Stress) Incontinence
Incidence
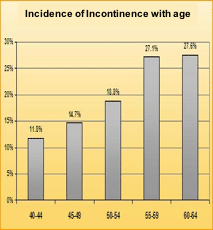
Urinary incontinence in women is a very common problem. One in three women will have some degree of incontinence in their lifetime. Stress incontinence occurs on exertion (running, bending), coughing or sneezing.
Stress incontinence is caused by weakness of the urethral sphincter (valve) and pelvic floor. Pregnancy, childbirth, menopause, previous surgery particularly hysterectomy and obesity all contribute to pelvic floor weakness and stress incontinence. Stress incontinence can also run in families.
Symptoms and signs
The degree of stress incontinence can vary considerably. For some women the leak is small and is managed by avoiding exertion and mapping toilets. For other women underwear changes and incontinence pads are a regular and distressing necessity. Some women are also aware of prolapse symptoms including bulging descent (a lump) of the vagina, dragging sensation and discomfort. Pelvic and low back pain can also be symptoms Mixed incontinence describes a combination of stress incontinence and urge incontinence symptoms (see Urge Incontinence) and the two causes of urinary leak are often seen together.Diagnostics
Your doctor will question you on your symptoms and your previous medical, surgical and obstetric history. An examination of your abdomen and pelvis will be a part of this assessment. All examinations are chaperoned by qualified nursing staff. You may be asked to complete questionnaires and fluid charts as part of your assessment. The gold standard investigation to assess incontinence is called a Urodynamic study. This involves the passage of a fine catheter into the bladder and rectum to measure pressures as the bladder fills and empties. The rectal catheter is used to subtract the abdominal pressure to give an accurate bladder reading. The urodynamic test is combined with Voiding Cytourethrography – Xray images – in order to get both pressures and pictures of your pelvic floor support. The urodynamic study takes approximately 30 minutes to perform and is not painful. Your consultant will give further details.

Fig 2 – X-ray picture showing bladder prolapse through the pelvic floor.
Treatment options
Pelvic Floor Exercises

Pelvic floor exercises help improve the tone (strengthen) the muscles of the pelvic floor. This helps to support the bladder and tighten around the bladder neck and urethra (water-pipe) during times of increased abdominal pressure (eg bending or running). Specific exercise can be taught to try and tighten the muscle. These exercises can be augmented by the use of vaginal cones (weights), biofeedback monitors or electrical stimulation. Pelvic floor exercises are taught by physiotherapists and need practised regularly at home to be effective. Pelvic floor exercises can improve stress incontinence in up to 70% of women, but only work if the exercises are continued.
More information about pelvic Floor Exercises can be found via the BAUS leaflets at BAUS and downloading the leaflet on Pelvic Floor Exercises (in women)
Bulking agents
More information on bulking injections can be found via the BAUS leaflet at BAUS and downloading the leaflet on Urethral Bulking
Mid urethral mesh slings (TVT and TVTO)
Mid urethral mesh procedures have been used since 1997. The procedures use a polypropylene mesh (plastic tape) around the urethra designed to act like a hammock, supporting the urethra and helping it to close more tightly when abdominal pressure is raised during coughing or exercising. The tape stays in place permanently.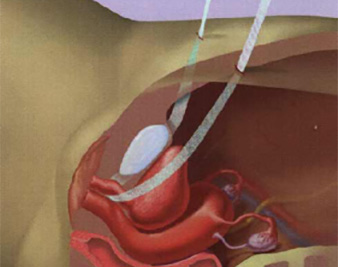
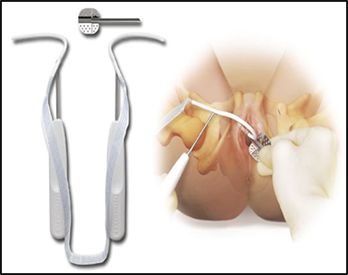
More information on TVT and TVTO procedure can be found via the BAUS leaflets at BAUS and downloading the leaflet on Synthetic mesh tape insertion (in women)
Awareness of mesh complications
More information on TVT and TVTO complications can be found via the BAUS leaflets at BAUS
Autologous rectus fascia slings
This operation works in a similar way to the TVT procedure (see Mid urethral mesh slings (TVT and TVTO) above). In this operation a sling is made from the tissues of abdominal wall and the sling is mounted on surgical sutures as a ‘sling on a string’ to be placed around the urethra. The procedure therefore needs both a vaginal and abdominal incision.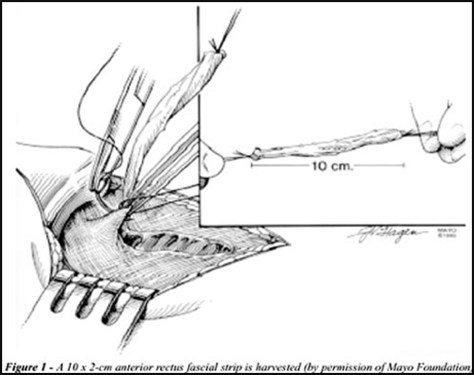
More information on Autologous rectus fascia slings can be found via the BAUS leaflets at BAUS and downloading the leaflet on autologous sling procedure for stress urinary incontinence in women.
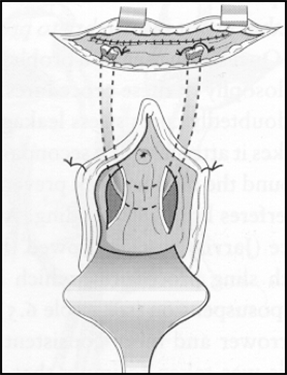
Colposuspension
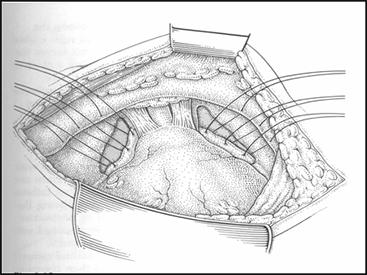
In this operation sutures are placed in the vagina either side of the bladder neck to elevate the bladder as a pelvic floor ‘face lift’. The operation corrects stress incontinence and prolapse simultaneously. Success rates are 80-90% although it can cause secondary prolapse of the bowel (rectocoele) in 1-8%. It is sometimes combined with a Sacrocolpopexy (see section on prolapse) to give complete pelvic floor support. Colposuspension can be performed through Bikini line ( Pfannensteil) incisions or keyhole (laparoscopic) incisions.
More information on Colposuspension can be found via the BAUS leaflets at BAUS and downloading the leaflet on Colposuspension for stress urinary incontinence (SUI).
Artificial urinary sphincter
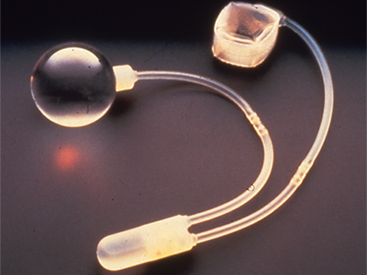
This surgery is usually reserved for women who have failed a primary (first) operation for stress incontinence. A plastic prosthesis – an artificial sphincter- is implanted to replace the function of the failed natural sphincter through an abdominal incision. The device is worked through a pump (button) system placed in the labia. Artificial urinary sphincters are successful in 80-90% of cases but risk erosion through the urethra (water pipe) or labia and infection in 10-20%. In such circumstances, they would have to be removed. The artificial sphincter lasts 10-15 years. More information on Artificial urinary sphincter can be found via the BAUS leaflets at BAUS and downloading the leaflet on Insertion of an artificial urinary sphincter (AUS) in women. A comparison of all the different options for female stress incontinence can be found at BAUS and downloading the leaflet COMPARISON OF TREATMENT OPTIONS FOR STRESS URINARY INCONTINENCE (SUI) IN WOMEN

